Ankylosing spondylitis (AS) is a chronic and often misunderstood condition that can drastically change how a person moves, stands, and feels.
One of the most visible and impactful changes it can cause is a forward head tilt—a posture where the head juts forward instead of sitting squarely above the shoulders.
This seemingly simple shift can lead to discomfort, pain, and challenges in daily activities.
But why does this happen?
What about AS causes this forward head posture? To answer this, we need to explore the nature of ankylosing spondylitis, how it affects the spine, and the body’s attempts to compensate.
This article by bestforwardheadposturefix unpacks the science, symptoms, and solutions behind forward head tilt in AS, guiding you through what’s happening inside the body and how people manage it.
This Article Covers:
- What Is Ankylosing Spondylitis?
- The Normal Anatomy and Posture of the Spine
- The Inflammatory Process in AS and Its Effects on the Spine
- Changes in Spinal Curvature and Mobility Caused by AS
- Why Forward Head Tilt Develops in AS: The Connection Explained
- How the Body Tries to Compensate: Postural Adjustments
- Real-Life Examples of Forward Head Tilt in People with AS
- The Consequences of Forward Head Tilt: Pain and Function
- Treatment and Management Strategies for Forward Head Tilt in AS
- Living with Forward Head Tilt: Tips for Daily Life
- Conclusion
What Is Ankylosing Spondylitis?
Ankylosing spondylitis is a type of inflammatory arthritis that primarily attacks the spine and the sacroiliac joints—the joints connecting the lower spine to the pelvis.
It typically begins in early adulthood and is more common in men than women.
The word “ankylosing” means stiffening, and “spondylitis” refers to inflammation of the vertebrae.
So, AS literally means inflammation that causes stiffness in the spine. AS is unique because it not only causes joint inflammation but also triggers new bone growth in the spine.
Over time, this new bone can bridge vertebrae together, leading to a rigid, fused spine. Imagine the flexible segments of your spine turning into a solid bone block—that is essentially what can happen in advanced AS.
The Normal Anatomy and Posture of the Spine
To understand how AS changes posture, it helps to know what a healthy spine looks like.
The spine has natural curves that help it absorb shock and maintain balance: The cervical spine (neck) curves slightly inward (lordosis), supporting the head’s weight and allowing it to move freely.
The thoracic spine (upper back) curves outward (kyphosis), forming the natural rounding of the upper back. The lumbar spine (lower back) curves inward again (lordosis), supporting the lower torso and pelvis. These curves keep your head balanced over your body.
When you look straight ahead, your ears should be roughly in line with your shoulders. This alignment minimizes strain on muscles and ligaments.
The Inflammatory Process in AS and Its Effects on the Spine
AS is driven by an autoimmune response, where the body’s immune system mistakenly attacks its own tissues, especially at the entheses—the points where ligaments and tendons attach to bone.
This leads to chronic inflammation, pain, and swelling.
Over time, inflammation causes damage, but the body attempts to repair this by laying down new bone. Key inflammatory molecules, like tumor necrosis factor-alpha (TNF-α) and interleukin-17 (IL-17), play a vital role in this process.
These molecules perpetuate inflammation and stimulate the abnormal bone growth that causes spinal fusion.
Changes in Spinal Curvature and Mobility Caused by AS
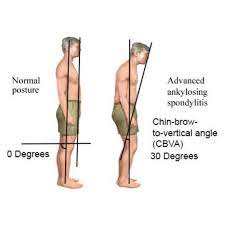
As AS progresses, the spine undergoes structural changes: The thoracic spine becomes more kyphotic—meaning it rounds forward more than usual, producing a hunched back.
The cervical spine, which should curve slightly inward to balance the head, loses this lordosis and may become straight or even curve forward (kyphotic). The vertebrae can fuse together, creating a rigid spine with very limited mobility.
This fusion and curvature reduce the spine’s flexibility and affect how the head and neck position themselves.
Why Forward Head Tilt Develops in AS: The Connection Explained
Forward head tilt occurs because the thoracic spine’s exaggerated kyphosis pushes the upper body forward.
Normally, the cervical spine would compensate by increasing its inward curve (cervical lordosis) to keep the head balanced over the shoulders and maintain a horizontal gaze.
However, in AS, the cervical spine is also stiffened due to inflammation, fusion, and new bone growth.
This limits the neck’s ability to extend backward and counteract the thoracic curve. As a result, the head shifts forward, leading to a characteristic “forward head posture” or “forward head tilt.”
To visualize this, think of a person with a hunched upper back trying to look straight ahead. If their neck cannot bend backward enough, the head must lean forward to keep the eyes level.
How the Body Tries to Compensate: Postural Adjustments?
The body strives to maintain balance and vision even when the spine’s shape changes drastically.
In AS, this means several compensatory mechanisms come into play: Forward head tilt helps keep the eyes looking forward despite the thoracic kyphosis. The jaw may jut forward to open the airway and maintain breathing.
The lower back and hips may adjust their position to stabilize the entire body. While these adaptations help maintain function, they also increase strain on muscles, ligaments, and joints.
The neck muscles work harder to hold the head up, often leading to fatigue and pain.
Real-Life Examples of Forward Head Tilt in People with AS
Consider John, a 35-year-old man diagnosed with AS five years ago. Initially, John noticed stiffness and mild pain in his lower back.
Over time, his upper back started to round forward, and he found himself tilting his head forward to see his computer screen clearly.
Despite exercises and medication, his neck became less flexible, and the forward head posture became more noticeable.
John’s forward head tilt caused neck pain and tension headaches, making his work and daily activities challenging.
Or take Maria, a 42-year-old woman with advanced AS. Her thoracic spine became severely kyphotic, and her neck lost much of its natural curve.
Maria’s forward head tilt made breathing feel more difficult, and she sometimes felt off-balance when walking. Her physical therapist focused on posture correction and strengthening her neck and upper back muscles to help reduce discomfort.
The Consequences of Forward Head Tilt: Pain and Function
Forward head tilt is not just a cosmetic concern—it has real effects on health and quality of life: Neck and shoulder pain occur as the muscles supporting the head become overworked and fatigued.
Headaches are common due to muscle tension and nerve irritation from poor posture. Reduced lung capacity follows as the chest’s forward collapse restricts lung expansion, making breathing less efficient.
Difficulty with balance and coordination arises because shifting the head forward moves the center of gravity, increasing fall risk.
Functional limitations develop, making simple tasks like driving, reading, or walking more difficult. These symptoms can compound, leading to reduced independence and emotional distress.
Treatment and Management Strategies for Forward Head Tilt in AS
While forward head tilt in AS can be challenging, several strategies can help manage the condition: Medications such as anti-inflammatory drugs, including NSAIDs and biologics targeting TNF-α or IL-17, reduce inflammation and slow disease progression.
Physical therapy tailored to improve spinal mobility, strengthen neck and upper back muscles, and teach posture awareness is critical.
Stretching helps maintain flexibility. Postural training and ergonomic adjustments, like using supportive chairs and adjusting computer screens to eye level, reduce strain.
Breathing exercises such as diaphragmatic breathing can counteract reduced lung capacity. Assistive devices like braces may support posture in severe cases. Rarely, surgery may be needed to correct severe spinal deformities.
Living with Forward Head Tilt: Tips for Daily Life
If you or a loved one has AS with forward head tilt, here are some practical tips: Maintain regular physical therapy and exercise routines.
Take frequent breaks during activities like working at a desk to stretch and reset posture. Use pillows and supports that encourage neck alignment during sleep. Stay mindful of head position during daily tasks; small corrections can add up.
Seek support groups or counseling to manage the emotional impact of chronic illness.
Takeaway
Ankylosing spondylitis causes forward head tilt through a complex interplay of inflammation, spinal fusion, and altered biomechanics.
The exaggerated thoracic kyphosis combined with stiffened cervical vertebrae prevents the neck from maintaining its natural curve, resulting in a fixed forward head posture.
This change in alignment leads to pain, functional limitations, and challenges in breathing and balance. However, understanding the underlying causes helps guide effective management.
With early diagnosis, appropriate medication, physical therapy, and lifestyle adjustments, people with AS can reduce the impact of forward head tilt and improve their quality of life.
If you notice changes in your posture or experience persistent neck pain, seeking medical advice early can make a significant difference.
By focusing on both the inflammatory process and postural effects, healthcare providers can offer comprehensive care that addresses the root of the problem and supports long-term well-being.
References: