Chiropractors play an essential role in correcting forward head posture (FHP) through targeted adjustments and posture-retraining techniques.
Forward head posture places significant stress on the cervical spine and surrounding muscles, resulting in chronic neck pain, headaches, muscle tension, and reduced range of motion.
Addressing this condition requires a combination of spinal adjustments, soft tissue therapy, and corrective exercises tailored to the patient’s needs.
Several studies, including those published in The Journal of Physical Therapy Science, highlight the effectiveness of chiropractic care in improving cervical alignment and alleviating symptoms associated with FHP.
This article compiled by BestForwardHeadPostureFix research team explores the specific techniques chiropractors use to address forward head posture and improve overall spinal health.
Points Covered in this Article
- Introduction
- Comprehensive Assessment and Diagnosis
- Postural Analysis
- Range of Motion Tests
- Palpation and Muscle Assessment
- Imaging Studies
- Spinal Adjustments
- How Adjustments Work
- Clinical Evidence Supporting Adjustments
- Soft Tissue Therapy for Muscle Balance
- Myofascial Release Therapy
- Trigger Point Therapy
- Cervical Traction and Spinal Decompression
- Cervical Traction Explained
- Clinical Evidence on Traction Therapy
- Postural Retraining and Corrective Exercises
- Common Corrective Exercises
- Benefits of Exercise-Based Posture Correction
- Complementary Therapies and Lifestyle Modifications
- Physical Therapy
- Massage Therapy
- Ergonomic Adjustments
- Frequent Movement Breaks
- Long-Term Management and Prevention
- Regular Chiropractic Check-Ups
- Core and Back Strengthening
- Body Awareness and Mindful Posture
- FAQs on Chiropractor for Fixing Text Neck
- Conclusion
Comprehensive Assessment and Diagnosis
The first step in correcting forward head posture is a thorough assessment to determine the extent of spinal misalignment. Chiropractors rely on a range of diagnostic tools and techniques to evaluate the patient’s condition accurately.
Step 1: Postural Analysis
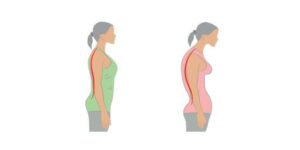
Chiropractors visually assess the patient’s posture from multiple angles to observe head position relative to the shoulders and spine. Forward head posture is characterized by the head jutting forward, causing the ears to sit in front of the shoulder line. This assessment helps determine the degree of misalignment.
Step 2: Range of Motion Tests
Patients are asked to perform neck movements such as flexion, extension, and rotation to check for any restrictions or pain. Limited range of motion is a common sign of FHP and can indicate muscle tightness or joint dysfunction.
Step 3: Palpation and Muscle Assessment
Chiropractors use palpation to feel for areas of muscle tension, joint stiffness, and spinal misalignment. Tight muscles in the neck and upper back, such as the upper trapezius and levator scapulae, are frequently associated with FHP.
Step 4: Imaging Studies
In some cases, X-rays or CT scans are used to provide a clearer picture of cervical spine alignment. These images help measure the degree of forward head positioning and rule out underlying conditions such as disc herniation or spinal degeneration.
Spinal Adjustments
Once the assessment is complete, chiropractors use spinal adjustments to restore the natural curve of the cervical spine and improve head posture. These adjustments are precise manipulations that target specific vertebrae to reduce joint restrictions and realign the spine.
According to a study published in The Journal of Manipulative and Physiological Therapeutics, spinal adjustments can significantly reduce pain and improve posture in patients with cervical spine dysfunction.
By addressing joint misalignments, chiropractors help relieve nerve pressure and promote proper head positioning.
How Adjustments Work:
- Reduce nerve irritation caused by misaligned vertebrae.
- Restore proper joint mobility in the cervical spine.
- Relieve muscle tension and improve blood flow to surrounding tissues.
Patients often experience immediate relief after adjustments, though consistent treatment is necessary for long-term results.
Soft Tissue Therapy for Muscle Balance
Soft tissue therapy is a crucial part of chiropractic care for forward head posture. Muscle imbalances are common in FHP, with tight muscles in the neck and chest and weak muscles in the upper back. Chiropractors use various soft tissue techniques to release tension and restore balance.
Myofascial Release Therapy:
This technique focuses on releasing restrictions in the fascia, the connective tissue surrounding muscles. Myofascial release helps reduce muscle tightness and improve flexibility, making it easier for patients to maintain proper posture.
Trigger Point Therapy:
Trigger points, or muscle knots, can develop in response to chronic tension.
Chiropractors apply targeted pressure to release these points, relieving pain and improving muscle function.
In severe cases, trigger point injections are used to reduce muscle pain.
Soft tissue therapy complements spinal adjustments by enhancing muscle elasticity and improving overall movement quality.
Cervical Traction and Spinal Decompression:
For patients with severe forward head posture or accompanying conditions such as disc compression, chiropractors may recommend cervical traction or spinal decompression therapy.
Cervical Traction:
Cervical traction gently stretches the neck, relieving pressure on the cervical vertebrae and discs. This therapy improves spinal alignment, reduces nerve compression, and promotes better blood flow to the affected areas.
Clinical Evidence:
A study in The Journal of Orthopaedic Research found that cervical traction can significantly improve neck pain and spinal alignment in patients with cervical spine disorders. For individuals with FHP, this therapy can help realign the head and reduce associated symptoms.
Postural Retraining and Corrective Exercises
In addition to spinal adjustments and soft tissue therapy, chiropractors emphasize the importance of posture retraining and corrective exercises.
These exercises strengthen weak muscles and help patients develop the muscle memory needed to maintain proper posture.
Common Corrective Exercises:
- Chin Tucks: Strengthen the deep cervical flexors and help retract the head into a neutral position.
- Wall Angels: Improve shoulder and upper back mobility, reducing tension in the thoracic spine.
- Scapular Squeezes: Strengthen the muscles between the shoulder blades, which are often weak in patients with FHP.
Regularly performing these exercises helps reverse muscle imbalances and promotes long-term postural correction.
Chiropractors often guide patients through these exercises during appointments and recommend a home routine for sustained results.
Complementary Therapies and Lifestyle Modifications
To achieve lasting improvements, chiropractors often incorporate complementary therapies and recommend lifestyle changes.
Physical Therapy:
Chiropractors may collaborate with physical therapists to develop a comprehensive treatment plan that combines chiropractic care with targeted strengthening and stretching exercises.
Massage Therapy:
Massage helps reduce muscle tension and improve circulation, making chiropractic adjustments more effective. It also promotes relaxation and pain relief.
Ergonomic Adjustments:
Chiropractors advise patients on improving workstation ergonomics, such as adjusting monitor height, using a chair with lumbar support, and maintaining a neutral head position during computer use.
These adjustments reduce strain on the neck and promote better posture throughout the day.
Frequent Movement Breaks:
Taking regular breaks from sitting or screen use helps prevent prolonged poor posture. Chiropractors often recommend setting reminders to stand, stretch, and reset posture throughout the day.
Long-Term Management and Prevention
Correcting forward head posture is not a one-time fix. Long-term management is essential to prevent recurrence and maintain proper alignment.
Regular Chiropractic Check-Ups:
Periodic visits to the chiropractor help monitor progress and address any emerging issues before they become chronic.
Core and Back Strengthening:
Strengthening the core and upper back muscles provides better support for the spine, reducing the risk of forward head posture returning.
Body Awareness and Mindful Posture:
Chiropractors encourage patients to develop body awareness and mindfulness about their posture, especially during activities like working at a desk or using electronic devices.
FAQs on Chiropractor for Fixing Text Neck
Q-1: How does a chiropractor measure forward head posture before treating it?
A-1: Expect objective checks, not just a glance. Common tools include the craniovertebral angle from side-view photos, a wall test (how far the head sits in front of the thorax), and simple tape/laser measurements from ear to shoulder. They’ll also screen breathing pattern, jaw motion, and thoracic mobility—because tight ribs and a clenched jaw often keep the head forward even after the neck is adjusted.
Q-2: What do chiropractic adjustments change in FHP—bones, muscles, or both?
A-2: The goal is to restore segmental motion where the neck and upper back are “stuck,” usually mid–lower cervical flexion and upper-thoracic stiffness. Gentle adjustments (or mobilizations) can free those segments so the head can come back over the shoulders without strain. Think of it as “re-centering the hinge” so muscles don’t have to tug constantly to hold you upright.
Q-3: Do chiropractors only adjust, or do they address tight/weak tissues that drive FHP?
A-3: They typically pair adjustments with soft-tissue work to the usual culprits—suboccipitals, SCM, upper traps, levator scapulae, and pec minor—plus rib mobilization to open the chest. Then they add activation for deep neck flexors and lower traps/serratus. A classic micro-sequence: suboccipital release → pec minor stretch at the doorway → 3×10 chin tucks with a towel roll → 2×10 wall slides.
Q-4: How does a chiropractor turn posture advice into a daily habit I’ll actually keep?
A-4: By creating “posture anchors.” Examples: a phone reminder every 45 minutes for a 60-second reset (neck stretches + 3 slow breaths); a monitor raised to eye level; keyboard pulled close so ribs don’t flare; and a backpack or cross-body bag to stop one-shoulder shrugging. They may also cue nasal, diaphragmatic breathing—each inhale should expand ribs sideways, not lift the shoulders.
Q-5: What progress timeline and checkpoints are realistic—and when is referral needed?
A-5: Many patients feel easier stacking within 2–4 weeks if they follow the homework; visible photo changes often appear by 6–8 weeks. Checkpoints: more chin-to-chest range, less end-of-day neck fatigue, and a growing craniovertebral angle on re-assessment photos. Red flags—progressive arm weakness, night pain, fever, recent trauma, or neurological changes—prompt co-management with a medical provider or imaging before continuing care.
Final Words
Chiropractors address forward head posture through a combination of spinal adjustments, soft tissue therapy, cervical traction, and posture retraining exercises.
Spinal adjustments help realign the cervical vertebrae, reducing nerve compression and restoring the neck’s natural curvature.
Soft tissue therapy releases tension in tight muscles, while cervical traction gently stretches the neck to alleviate pressure on spinal discs and nerves.
Posture retraining exercises, such as chin tucks and scapular squeezes, strengthen weakened muscles and promote long-term correction.
Complementary therapies like massage, physical therapy, and ergonomic adjustments further enhance recovery and help prevent relapse.
Studies published in The Journal of Manipulative and Physiological Therapeutics confirm the effectiveness of chiropractic care in improving cervical spine alignment and reducing chronic pain caused by forward head posture.
If you struggle with forward head posture, consulting a chiropractor can be a highly effective step toward recovery.
Consistent care, combined with lifestyle adjustments and a proactive approach to posture management, can significantly improve your spinal health, reduce pain, and enhance your overall quality of life.
References: