Neck pain can feel like a fire alarm that never shuts off, especially when tiny cervical joints or irritated nerve roots keep fueling inflammation.
Cortisone injections, when targeted precisely, help quiet that alarm right where it starts instead of blanketing your whole body with pills.
They switch off inflammatory chemicals quickly, then reset the genes that keep inflammation brewing, giving tissues a chance to calm down.
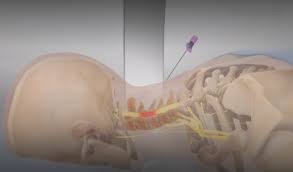
Modern imaging means the medicine can be placed with millimeter-level accuracy at the facet joint, around the medial branch nerve, or in the epidural space.
As per BestForwardHeadPostureFix, “Relief isn’t magic—it’s biology—so pairing the shot with smart rehab is the real secret to lasting results”.
Below is the clear, step-by-step “how it works,” plus what to expect before, during, and after the procedure.
Index
- Step 1: What “cortisone” actually is in the neck
- Step 2: Where inflammation lives in cervical pain
- Step 3: The deep genomic pathway (how genes get reset)
- Step 4: The fast, non-genomic effects (why some relief is quick)
- Step 5: Choosing the target—facet, medial branch, or epidural
- Step 6: Formulation and safety essentials that matter
- Step 7: What benefit typically looks like (timeline and durability)
- Step 8: From prep to aftercare—your injection playbook
- Step 9: Who should pause or avoid injections
- Step 10: Turning short-term relief into long-term gains
- Conclusion: Using cortisone shots wisely—precise, practical, and part of a plan
Step 1: What “Cortisone” Actually is in the Neck
“Cortisone shot” is the everyday term for a corticosteroid injection—most commonly dexamethasone, betamethasone, methylprednisolone, or triamcinolone.
If cortisone itself is used, local enzymes convert it to cortisol, the active form that binds glucocorticoid receptors inside cells.
Once bound, that receptor heads to the cell nucleus and starts re-programming inflammation.
This is why steroid placed right at the irritated joint capsule or nerve sleeve can outperform general painkillers for focused problems: it delivers the anti-inflammatory signal at the source.
Step 2: Where Inflammation Lives in Cervical Pain?
Two neighborhoods in the neck are common culprits.
First are the facet (zygapophyseal) joints—small, synovial joints that can develop synovitis and capsular swelling, especially with arthritis or micro-strain from posture.
Second is the nerve root sleeve and nearby epidural space, where a bulging disc or bony narrowing can bathe the nerve in inflammatory molecules like cytokines and prostaglandins.
Both situations create a loop: inflammation sensitizes nerves, sensitized nerves provoke more guarding and micro-trauma, and the cycle repeats.
A well-placed steroid quiets the chemical drivers so the loop can unwind.
Step 3: The Deep Genomic Pathway (how Genes get Reset)
Inside inflamed cells, the steroid–receptor complex moves into the nucleus and dials down genes that crank out inflammatory proteins (think cytokines and chemokines) while dialing up genes that promote resolution.
A standout is annexin A1, which helps block phospholipase A2, the enzyme that releases arachidonic acid—the raw material for prostaglandins and leukotrienes.
By choking off that supply line, cortisone reduces tissue swelling, pressure inside a cramped joint capsule or foramen, and the chemistry that keeps local nerves jumpy.
Step 4: The Fast, Non-Genomic Effects (why some Relief is Quick)
Not all of the benefit waits on gene changes. Some steroid effects happen within minutes by acting at cell membranes and ion channels.
These non-genomic actions stabilize irritable nerve membranes and modulate neurotransmitter release, often softening sharp, radiating pain early on.
The quick calm is then “handed off” to the slower genomic effects that make relief more durable over days to weeks.
Step 5: Choosing the Target—Facet, Medial Branch, or Epidural
@ Intra-articular facet joint injection. If your main complaint is axial neck pain that localizes to one side and flares with extension/rotation, the facet joint itself may be the source.
A small volume of anesthetic and steroid is placed inside the joint capsule to reduce synovitis.
@ Medial branch block. The tiny medial branch nerves carry pain from the facet joints. An injection around these nerves can be used diagnostically (to confirm the joint as the pain generator) and, at times, therapeutically.
When pain relief after properly controlled medial branch blocks is clear and reproducible, radiofrequency ablation may be considered for longer-term benefit.
@ Cervical epidural steroid injection. When arm pain, tingling, or weakness suggest nerve root irritation from a disc or foraminal stenosis, the target becomes the epidural space.
The interlaminar route spreads medication more broadly; the transforaminal route delivers closer to a single, inflamed nerve root. Selection depends on your symptoms, imaging, and the treating clinician’s expertise.
Step 6: Formulation and Safety Essentials that Matter
Particle size matters in the neck. For cervical transforaminal injections, clinicians increasingly favor non-particulate steroids such as dexamethasone to reduce the already rare risk of vascular entry and embolic complications.
Regardless of approach, real-time imaging and contrast testing help confirm safe needle placement before the steroid goes in.
Dose is kept as low as reasonably effective, and there is no automatic “series of three” unless a single injection shows clear functional value.
Step 7: What Benefit Typically Looks Like (Timeline and Durability)
Relief commonly follows a two-phase curve.
Phase one is the local anesthetic “preview” that can ease pain within hours but wears off by the next day.
Phase two is the steroid effect, which typically builds over 24–72 hours as inflammatory cascades shut down.
Many people enjoy meaningful relief for several weeks to a few months; in selected cases, benefit lasts longer, especially when the underlying driver is treated (for example, by improving posture mechanics or addressing a reversible irritation).
Because long-term results vary, it’s wise to track pain scores and function milestones so decisions about repeating or moving on to other options are data-driven.
Step 8: From Prep to Aftercare—Your Injection Playbook
Here are a three stages:
Before the Procedure:
- Nail the diagnosis. History, exam, and imaging should all point to a likely pain generator (facet vs. nerve root). This reduces “scatter” and improves the odds that a single, precisely targeted injection will help.
- Align the target and route. Your clinician will choose intra-articular facet, medial branch, interlaminar epidural, or transforaminal epidural based on your pattern of symptoms.
- Medication check. Anticoagulants, antiplatelets, and bleeding risks must be coordinated. Active infection or uncontrolled blood sugar are reasons to postpone.
- The goal is to reduce inflammation enough to unlock movement and rehab—not to act as a stand-alone cure.
During the Procedure:
5) Imaging guidance. Ultrasound or fluoroscopy is used to guide the needle; a small amount of contrast is injected to confirm the tip is in a safe, intended space.
6) Small dose, big impact. A tiny volume of steroid plus local anesthetic is placed precisely at the target, minimizing systemic exposure.
After the Procedure:
7) Short observation. You’ll be monitored briefly, then discharged with simple activity guidance.
8) Sugar watch if diabetic. Expect a temporary rise in blood glucose for a few days; plan monitoring and medication adjustments with your clinician.
9) Rehab window. Use the “quieted” period to restore deep neck flexor strength, scapular control, and movement confidence.
10) Track the win. Keep a simple diary of pain scores, sleep quality, desk tolerance, and turning/looking-over-shoulder range so the next step is obvious.
Step 9: Who should Pause or Avoid Injections
Absolute or relative “not now” signals include active infection, uncontrolled bleeding risk, uncontrolled diabetes, allergy to planned medications or contrast, and progressive neurologic deficits that need urgent evaluation.
Pregnancy, severe osteoporosis at the target, or recent steroid exposure elsewhere may also prompt a rethink of timing or dosage.
None of these are automatic “no,” but they do require a thoughtful, individualized risk–benefit discussion.
Step 10: Turning Short-Term Relief into Long-Term Gains
A cortisone shot opens a door; you still have to walk through it.
In practical terms, that means pairing the injection with posture fixes (monitor height, chair support, frequent micro-breaks), mobility resets (gentle nerve glides if radicular symptoms are present), and progressive strengthening (deep neck flexors, mid-back, and rotator cuff).
Many people also benefit from sleep-position tweaks—a pillow that supports neutral cervical alignment and avoids prolonged end-range rotation.
The more you do to remove the mechanical spark, the less often chemistry needs to step in.
Takeaway: Using Cortisone Shots Wisely—Precise, Practical, and Part of a Plan
Cortisone injections don’t merely mask neck pain—they reduce the very chemistry that keeps tissues swollen and nerves irritable, giving your cervical spine a chance to reset.
The real magic is in precision: the right target, the right route, and meticulous image guidance to place a small dose exactly where it will count.
Because benefit is often short-to-medium term, the smartest play is to use that window to rebuild strength and movement patterns so relief lasts longer than the medicine itself.
Formulation details matter too; non-particulate options and careful contrast testing add layers of safety without sacrificing effectiveness.
If you live with diabetes or other medical conditions, plan ahead for short, predictable ripple effects—like a temporary glucose bump—and keep your care team in the loop.
Track your response with simple, functional benchmarks so decisions about repeating or escalating care are grounded in what actually improved your life.
Above all, see the injection as a bridge—not the destination—linking today’s relief to tomorrow’s stronger, more confident neck.
Used thoughtfully, a targeted cervical cortisone injection can quiet the fire, restore motion, and help you return to the activities that make you feel like yourself again.
References:
