Cervical fusion surgery is a critical procedure designed to restore stability and alignment in the neck.
It is commonly used to treat conditions such as cervical spondylosis, herniated discs, and spinal instability caused by trauma or degeneration.
This article will explore the mechanics of cervical fusion surgery, its role in stabilizing neck alignment, the benefits and risks, and real-life examples to illustrate its effectiveness.
By delving into the “how” and “why” of cervical fusion surgery, we aim to provide a comprehensive understanding of its role in neck health.
Index
- Understanding Cervical Fusion Surgery
- The Mechanics of Cervical Fusion Surgery
- How Cervical Fusion Stabilizes Neck Alignment
- Conditions That Require Cervical Fusion Surgery
- Benefits of Cervical Fusion Surgery
- Potential Risks and Considerations
- Real-Life Example: Jane’s Recovery Journey
- Scientific Evidence Supporting Cervical Fusion Surgery
Understanding Cervical Fusion Surgery
Cervical fusion surgery is a specialized procedure aimed at permanently joining two or more vertebrae in the neck to eliminate movement between them.
This surgical intervention is often necessary to address conditions such as cervical instability, herniated discs, degenerative disc disease, or traumatic injuries.
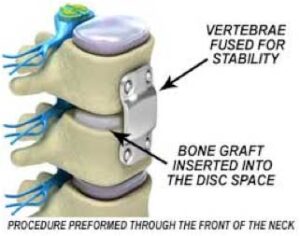
The procedure involves the use of bone grafts, which may be harvested from the patient (autografts) or obtained from a donor (allografts).
These grafts are strategically placed between the affected vertebrae to promote the natural process of bone fusion.
Additionally, metal hardware, including screws, rods, or plates, is used to secure the vertebrae in place during the healing process, ensuring stability and alignment.
By removing movement at the problematic site, cervical fusion surgery not only alleviates pain caused by nerve compression and instability but also prevents further degeneration or damage.
The primary objective is to stabilize the neck, restore alignment, and improve the patient’s overall quality of life.
The Mechanics of Cervical Fusion Surgery
Cervical fusion surgery follows a structured process to ensure precision and effective results:
- Preparation: Advanced imaging techniques, such as MRI or CT scans, are utilized to pinpoint the affected vertebrae and plan the surgical approach.
- Bone Grafting: Bone grafts are inserted between the vertebrae to facilitate the fusion process. These grafts may be autografts, taken from the patient’s own body, or allografts, sourced from a donor.
- Implant Placement: To stabilize the vertebrae during the healing phase, surgeons use metal hardware, including screws, rods, and plates. These implants hold the vertebrae firmly in place, ensuring proper spinal alignment.
- Healing Process: Over the course of several months, the bone grafts integrate with the surrounding vertebrae, forming a single, solid structure. This natural fusion eliminates movement between the affected vertebrae, reducing pain and improving neck stability.
This carefully orchestrated process ensures the neck is stabilized, misalignment is corrected, and the patient experiences long-term relief from their symptoms.
How Cervical Fusion Stabilizes Neck Alignment
Eliminating Abnormal Motion: Cervical fusion removes the mobility of unstable vertebrae, which can contribute to misalignment. By securing these vertebrae, the procedure prevents abnormal motion and restores proper posture.
Redistributing Spinal Load: Spinal instability often leads to uneven load distribution, which can exacerbate misalignment. Fusion surgery ensures that the remaining vertebrae bear weight more evenly, promoting overall spinal health.
Preventing Further Degeneration: Conditions like degenerative disc disease can worsen neck alignment over time. By stabilizing the spine, cervical fusion halts this progression.
Realignment: For patients with scoliosis or kyphosis affecting the cervical spine, fusion can correct the curvature, improving both function and aesthetics.
Conditions That Require Cervical Fusion Surgery
Cervical fusion surgery is commonly used to address a variety of neck conditions that cause instability and misalignment. Key indications include:
- Cervical Spondylosis: Degenerative changes in the cervical discs and joints can lead to instability and misalignment of the spine. Fusion surgery stabilizes the affected vertebrae, reducing pain and preventing further degeneration.
- Herniated Discs: When cervical discs herniate, they can compress nerves and destabilize the neck. In such cases, the herniated disc is often removed, and fusion is performed to restore stability and maintain proper alignment.
- Traumatic Injuries: Fractures or dislocations in the cervical spine caused by accidents or falls frequently necessitate fusion surgery. The procedure prevents further damage, stabilizes the spine, and realigns the vertebrae.
- Spinal Deformities: Conditions such as cervical kyphosis (forward curvature) or scoliosis (lateral curvature) can cause significant misalignment and functional impairment. Fusion surgery corrects these deformities and helps restore neck function.
- Cervical Instability: This condition, often caused by rheumatoid arthritis or other disorders, leads to pain, misalignment, and reduced mobility. Fusion surgery stabilizes the spine, alleviating symptoms and preventing further complications.
These scenarios highlight the critical role cervical fusion surgery plays in addressing diverse causes of neck instability and restoring alignment.
Benefits of Cervical Fusion Surgery
Improved Stability: By fusing unstable vertebrae, the procedure ensures that the neck remains aligned during movement.
Pain Relief: Fusion alleviates pain caused by nerve compression and joint instability, improving the patient’s quality of life.
Enhanced Functionality: Patients often regain mobility and strength in their upper body following surgery.
Reduced Risk of Further Injury: Stabilizing the neck protects the spinal cord and nerves from additional damage.
Correction of Deformities: Fusion addresses abnormal curvatures, such as scoliosis or kyphosis, enhancing posture and spinal health.
Potential Risks and Considerations
While cervical fusion surgery is generally safe, it is not without risks. Patients should consider the following:
Reduced Neck Mobility: Fusing vertebrae limits the range of motion in the neck, which may affect daily activities.
Adjacent Segment Disease: Fusion increases stress on adjacent vertebrae, potentially leading to degeneration over time.
Infection and Hardware Issues: Surgical complications, including infections or hardware failure, can occur, though they are rare.
Recovery Challenges: The healing process requires several months, during which patients must follow strict guidelines to ensure proper fusion.
Long-Term Implications: Patients may need ongoing physical therapy to adapt to changes in neck mobility.
Real-Life Example: Jane’s Recovery Journey
Jane’s Background:
Jane, a 45-year-old accountant, began experiencing severe neck pain, stiffness, and tingling sensations radiating down her arms. These symptoms were significantly affecting her daily life, including her ability to work comfortably. An MRI revealed a herniated cervical disc and instability between her C5 and C6 vertebrae, causing nerve compression and misalignment.
The Surgery:
After consulting with her spine specialist, Jane opted for cervical fusion surgery to address her condition. During the procedure, her surgeon removed the herniated disc and replaced it with a bone graft to promote fusion. Metal plates and screws were inserted to stabilize the vertebrae and maintain alignment while the bone healed.
The Recovery:
In the weeks following surgery, Jane experienced initial discomfort and had to adapt to reduced neck mobility. However, with a structured physical therapy program, she gradually regained strength and flexibility. By six months, Jane reported significant pain relief, no tingling in her arms, and noticeable improvement in her posture.
Outcome:
Jane’s story illustrates how cervical fusion surgery can successfully restore neck stability and alleviate symptoms caused by severe misalignment. Her improved quality of life underscores the procedure’s effectiveness in managing debilitating neck conditions.
Scientific Evidence Supporting Cervical Fusion Surgery
Numerous studies validate the efficacy of cervical fusion surgery in stabilizing neck alignment:
Study in The Spine Journal A 2020 study demonstrated that cervical fusion significantly reduced pain and improved spinal stability in patients with degenerative disc disease.
Research in Clinical Spine Surgery A 2018 review found that fusion corrected deformities in 90% of patients with cervical kyphosis, showcasing its effectiveness in realignment.
Long-Term Outcomes A study published in the Journal of Neurosurgery: Spine reported that patients experienced sustained improvements in neck alignment and function five years post-surgery.
Conclusion
Cervical fusion surgery is a vital intervention for stabilizing neck alignment in patients with spinal instability or deformities.
By eliminating abnormal motion, redistributing spinal loads, and preventing further degeneration, it restores function and alleviates pain.
While the procedure has risks, careful planning and adherence to postoperative care ensure successful outcomes.
Through case studies like Jane’s, we see how fusion surgery can transform lives, emphasizing its importance in modern spine care.
References: