Have you ever wondered if that persistent neck stiffness could be a sign of something more?
Or why your chiropractor tilts your head, takes measurements, and sometimes even sends you for an X-ray before starting treatment?
Cervical misalignment is not just about a bone being “out of place” — it is about how your neck’s structure, movement, and nerve function work together.
In this article, we shall uncover the exact steps chiropractors take to assess the neck, from your first conversation in the clinic to advanced posture analysis and neurological testing.
You shall find out when imaging is truly necessary, how range of motion is measured with precision tools, and why palpation has both value and limits.
Best Forward Head Posture Fix research team would also explore how outcome measures track your recovery.
By the end, you would know exactly what happens during an assessment — and why it is more scientific than you might think.
Article Index
- What “cervical misalignment” actually means (and why words matter)
- Step 1: History taking that maps the problem (not just the pain)
- Step 2: Safety first — screening for red flags and vascular/ligament risks
- Step 3: Visual posture and movement checks (what the eyes can see)
- Step 4: Measuring cervical range of motion the right way
- Step 5: Neurological exam for possible nerve‐root involvement
- Step 6: Orthopedic provocation tests (and what their results really mean)
- Step 7: Palpation and segmental motion testing — useful, but with limits
- Step 8: When imaging helps (and exactly how chiropractors read it)
- Step 9: Outcome measures that quantify “how much better”
- Pulling it all together: The chiropractor’s clinical reasoning loop
- Your practical solution: What you can do this week
What “Cervical Misalignment” actually Means (and Why Words Matter)
When people hear “misalignment,” they often picture a bone sitting out of place.
Clinically, chiropractors mean something more precise: a spinal segment that’s stiff, irritated, poorly coordinated, or showing abnormal curvature that could be contributing to symptoms.
They focus on dysfunctions that can be influenced by treatment rather than just “straightening things out.”
Assessment blends safety checks, measurable range of motion, neurological findings, specific orthopedic tests, and sometimes imaging.
The goal is to identify what is changeable and track improvements over time, not chase a mythical “perfect” neck.
Step 1: History Taking that Maps the Problem (Not just the Pain)
The conversation comes first.
Chiropractors ask about when symptoms began, whether they appeared after trauma or gradually, how they behave over 24 hours, and what makes them better or worse.
They shall map your pain pattern—whether it’s neck-only, radiates into the shoulder, or travels into the arm or hand.
They also explore work and recreational activities, past injuries, sleep habits, and medical history.
These details help form early hypotheses and uncover “yellow flags” like anxiety about movement, which can influence recovery.
Step 2: Safety First — Screening for Red Flags and Vascular/Ligament Risks
Before any hands-on work, chiropractors screen for serious but rare conditions. These include suspected fractures, infections, cancer, or vascular problems.
They also check for ligament instability in the upper cervical spine, especially after trauma. Tools like clinical decision rules and guidelines help decide if imaging is needed early.
This step ensures that treatment is safe and that any red-flag findings are referred for medical care.
Step 3: Visual Posture and Movement Checks (what the Eyes can See)
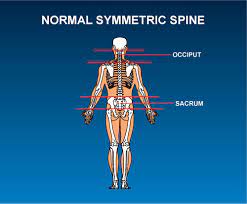
A cervical spine posture assessment checklist guides visual analysis.
The chiropractor looks for forward head posture, rounded shoulders, and uneven shoulder height.
They watch how you move—whether you avoid turning your head fully or compensate with the upper back.
They may ask you to mimic real-world tasks like checking your blind spot while driving.
The visual and functional clues help link postural habits with your symptoms.
>>> Want to Learn How I Treated My Forward Head Posture at Home??? Click Here to Find Out! <<<
Step 4: Measuring Cervical Range of Motion the Right Way
Good clinicians don’t just “eyeball” neck movement—they measure it.
Tools like the CROM device cervical range of motion, dual inclinometers, or validated mobile apps quantify flexion, extension, side-bending, and rotation.
Some even measure upper cervical motion separately.
These devices produce consistent, repeatable results, making it easier to track genuine improvement rather than relying on guesswork.
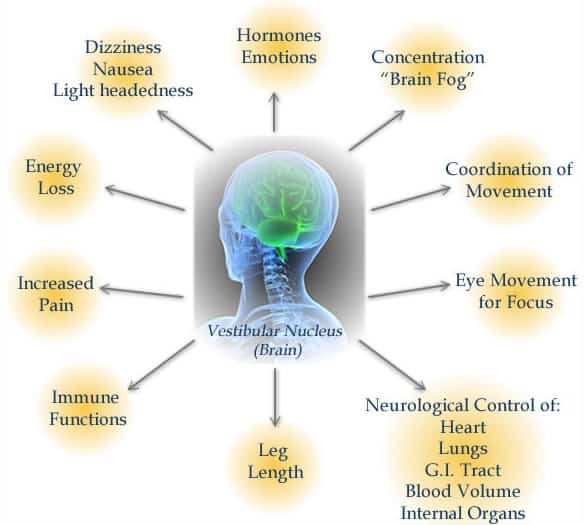
Step 5: Neurological Exam for Possible Nerve-Root Involvement
If symptoms suggest nerve irritation, a neurological exam for cervical radiculopathy is done.
This includes testing skin sensation in dermatomal patterns, muscle strength in specific myotomes, and reflexes in the biceps, brachioradialis, and triceps.
Sometimes upper motor neuron signs are also checked. These tests help confirm whether nerve roots are affected and guide treatment planning.
Step 6: Orthopedic Provocation Tests (and what their Results Really Mean)
Special tests can provide clues:
- Spurling’s test may reproduce nerve root pain when the neck is side-bent and compressed.
- Neck distraction may ease symptoms, suggesting nerve root decompression helps.
- Upper limb neurodynamic tests check how nerve tissue responds to movement.
Chiropractors rarely rely on one test alone—they use clusters of results plus your history to decide whether nerve compression is likely.
Step 7: Palpation and Segmental Motion Testing — Useful, but with Limits
Chiropractors feel along the neck for tenderness, tight muscles, and stiff joints.
Segmental motion palpation is meant to detect restricted spinal levels, but research shows mixed results for inter-examiner consistency.
This is why reliability of motion palpation in chiropractic is considered moderate at best—it works better as supporting evidence rather than the main decision-maker.
Palpation findings are most valuable when paired with measurable changes after treatment.
Step 8: When Imaging Helps (and Exactly how Chiropractors Read it)
Knowing when do chiropractors order cervical x rays is key: after significant trauma, with severe or worsening neurological symptoms, or when structural issues must be ruled out before treatment.
MRI is preferred for suspected nerve or spinal cord issues, CT for fractures, and X-rays for bony alignment or instability.
When X-rays are used, chiropractors often measure spinal curves using methods like the Cobb angle or posterior tangent method, which are consistent and reproducible.
Step 9: Outcome Measures that Quantify “How much Better?”
Beyond pain scales, the Neck Disability Index (NDI) is widely used to measure how neck pain affects daily activities like driving, reading, and sleeping. It is reliable, easy to score, and sensitive to change. Regularly tracking NDI scores alongside range-of-motion measures helps show if treatment is making a meaningful difference.
Pulling it all Together: The Chiropractor’s Clinical Reasoning Loop
The process flows logically:
- Rule out dangerous conditions and decide if imaging is needed.
- Build a working hypothesis from history, posture, and movement patterns.
- Collect measurable baselines from motion devices, neuro exams, and orthopedic tests.
- Apply selective hands-on techniques or exercise, and immediately reassess to see what works.
- Track progress with the same tools used at baseline, adjusting the plan if needed.
Example: Priya’s Assessment
Priya, a graphic designer, has right-sided neck pain and occasional tingling in her forearm.
- History shows long laptop hours and symptom relief at night.
- Safety screening clears serious issues.
- Posture check finds forward head and rounded shoulders.
- A CROM device shows reduced rotation to the right.
- Neuro exam reveals mild wrist extensor weakness and a reduced triceps reflex.
- Spurling’s test is mildly positive; nerve tension testing reproduces tingling.
The plan: ergonomic changes, targeted mobilization, nerve-gliding exercises, and a review in four weeks—imaging only if no progress.
What You’ll Actually Experience in the Clinic?
- A conversation-heavy start to gather your story.
- Brief safety checks for red flags.
- Measured movement tests rather than guesswork.
- Targeted, gentle hands-on treatment matched to your comfort.
- Simple, specific home exercises.
- Regular outcome tracking to prove improvement.
Myths that Deserve Busting
- A neck “crack” means it’s fixed. Not necessarily; relief can happen without a pop.
- Everyone needs X-rays. Not true—imaging is based on clear clinical indicators.
- Palpation tells the whole story. It’s useful, but not reliable enough on its own.
Your Practical Solution: What You can do this Week?
- Bring a symptom map to your appointment—note where pain travels and what triggers it.
- Ask for measurable baselines like ROM and NDI scores.
- Try two gentle self-checks at home: short towel traction and chin-in head turns.
- Fix your setup—raise screens, hold your phone at eye level, and take micro-breaks.
- Agree on a review point—if there’s no progress in 4–6 weeks, revisit the plan.
- Track both symptoms and function so you and your chiropractor can see what’s working.
Final Word
Understanding how chiropractors assess cervical misalignment takes the mystery out of the process.
It is not about chasing a single “out” bone—it is about systematically ruling out serious problems, finding movement or control issues that matter, applying safe interventions, and proving you are getting better with measurable results.
When you know the steps, you can be an active partner in your own care.
References: