Forward head posture (FHP) is a common condition in today’s technology-driven world, often resulting from prolonged screen time and poor ergonomics.
Assessing neck alignment is critical for diagnosing FHP, understanding its impact on the body, and developing effective interventions.
In this article BestForwardHeadPostureFix will explore various methods used to evaluate neck alignment, discuss how to fix hunchback, why such assessments are essential, and how they inform treatment plans.
Index
- Understanding Forward Head Posture and Its Implications
- The Importance of Assessing Neck Alignment
- Tools and Techniques for Measuring Neck Alignment
- Step-by-Step Evaluation Methods
- Common Symptoms Identified Through Assessment
- Real-Life Example: John’s Neck Alignment Evaluation
- Scientific Backing for Neck Alignment Assessments
- Conclusion: The Value of Proper Assessment in Addressing FHP
A Quick Look at FHP and Its Implications
Forward head posture (FHP) is a condition where the head shifts excessively forward in relation to the body’s midline.
This abnormal positioning places undue stress on the neck and shoulders, significantly impacting musculoskeletal health.
The cervical spine and supporting muscles bear increased load as the head moves forward, with each inch of displacement adding approximately 10 pounds of additional strain, according to a study in the Journal of Physical Therapy Science.
This strain leads to chronic pain, stiffness, and tension headaches.
Over time, FHP can trigger compensatory changes such as rounded shoulders and exaggerated thoracic kyphosis, further destabilizing the body’s alignment.
These cascading effects emphasize the importance of early identification and intervention.
Neck alignment assessments are critical in determining the severity of FHP and developing tailored rehabilitation plans.
Addressing FHP not only alleviates symptoms but also improves overall posture and quality of life.
The Importance of Assessing Neck Alignment
A thorough evaluation of neck alignment is more than just a clinical formality—it is the foundation of any effective strategy to correct forward head posture (FHP).
Without a detailed assessment, practitioners are essentially guessing, which can lead to incomplete recovery or even worsening of symptoms.
Here is why proper neck alignment assessment is so critical:
Determining Severity of Misalignment:
Quantifying the extent of FHP helps set realistic goals and guides treatment intensity. A commonly used metric is the Craniovertebral Angle (CVA), measured using side-view photographs or X-rays.
A CVA less than 50° usually indicates moderate to severe forward head posture. A 2021 study published in Physical Therapy Science found a direct correlation between CVA and neck pain intensity, making it a valuable diagnostic tool.
Identifying Underlying Causes:
Assessment reveals what’s driving the poor posture. Is it tight sternocleidomastoid muscles? Weak deep neck flexors? Joint subluxation such as hip joint stress? Habitual phone use?
For instance, a desk worker with weak scapular stabilizers may unknowingly perpetuate FHP daily. Understanding these factors ensures that therapy targets the root problem—not just the symptoms.
Creating Personalized Treatment Plans:
A chiropractor or physical therapist uses assessment data to develop a highly individualized care plan. Someone with minor postural deviation may need only home exercises and ergonomic adjustments, whereas a severe case with joint restrictions might require manual therapy and neuromuscular re-education.
Monitoring Progress Over Time:
Objective re-assessments—such as postural photographs, goniometric measurements, or digital motion analysis—help determine whether the interventions are working. If CVA improves and symptoms decrease, it’s a win. If not, it is time to adjust the plan.
Ultimately, a structured evaluation transforms posture correction into a data-driven process. It ensures that every stretch, adjustment, and exercise is part of a targeted, measurable strategy—maximizing recovery and minimizing trial-and-error.
Tools and Techniques for Measuring Neck Alignment
A variety of tools and techniques are used to assess neck alignment and identify the severity of forward head posture (FHP).
These include:
- Plumb Line Test
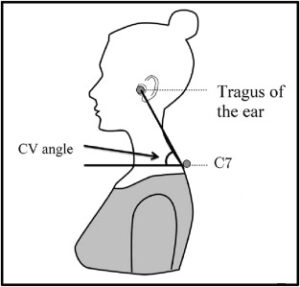
The plumb line test is a straightforward method where a string is aligned vertically with the body. In proper posture, the ear should align with the shoulder. Any forward displacement of the ear indicates FHP. - Craniovertebral Angle (CVA)
CVA is measured using a goniometer or digital tools. It evaluates the angle between the horizontal plane and a line from the ear’s tragus to the C7 vertebra. A smaller CVA correlates with more severe FHP. - Digital Posture Analysis
Modern tools such as mobile apps and posture analysis software capture and analyze side-profile images or videos, providing precise measurements of neck alignment. - Range of Motion (ROM) Tests
ROM tests assess the flexibility and mobility of the neck, identifying restrictions and stiffness associated with FHP. - Palpation
Physical examination through palpation detects muscle tension, stiffness, or abnormalities in the cervical spine and surrounding areas.
These techniques together provide a comprehensive understanding of FHP, aiding in accurate diagnosis and treatment planning.
Step-by-Step Evaluation Methods
- Initial Observation
The assessment begins with the patient standing naturally while the therapist conducts a visual examination. Key observations include:- The head’s position relative to the shoulders.
- Any asymmetry in the height of the shoulders or neck.
- Spinal curvature, especially in the cervical and thoracic regions, to identify excessive kyphosis or lordosis.
- Plumb Line Assessment
The patient is positioned near a plumb line to check for deviations. The therapist evaluates whether the ear aligns vertically with the acromion process (shoulder tip). Misalignment indicates the degree of forward displacement. - Craniovertebral Angle Measurement (CVA)
Using a goniometer, the therapist measures the craniovertebral angle. The angle is formed by a horizontal line from the C7 vertebra and a line connecting C7 to the ear tragus. A CVA below 50° is indicative of forward head posture. - Dynamic Movement Testing
The patient performs neck movements, such as tilts, rotations, and forward extensions. Restricted or uneven motion signals potential muscle imbalances, joint stiffness, or both. - Palpation of the Cervical Spine
Through touch, the therapist examines the cervical vertebrae and adjacent muscles for tightness, tenderness, or misalignment. This tactile evaluation provides insights into muscle tension and joint dysfunction.
These steps collectively provide a comprehensive understanding of FHP, enabling therapists to identify underlying causes and severity levels.
Common Symptoms Identified Through Assessment
Evaluating neck alignment often uncovers a range of symptoms directly associated with forward head posture (FHP). These include:
- Neck Pain and Stiffness: Prolonged strain on cervical muscles leads to discomfort and tightness.
- Tension Headaches: Misalignment in the upper cervical spine often triggers tension headaches due to increased pressure on surrounding structures.
- Reduced Neck Mobility: Tightened muscles and joint stiffness impair the neck’s ability to move freely in different directions.
- Shoulder and Upper Back Pain: Compensatory postural adjustments, such as rounded shoulders, place strain on the upper back and shoulders.
- Jaw Pain: Dysfunction of the temporomandibular joint (TMJ), commonly linked to FHP, causes pain and limited jaw movement.
Identifying these symptoms during the assessment phase allows therapists to determine the severity of FHP and understand its impact on the patient’s overall musculoskeletal health.
Early recognition ensures targeted and effective intervention.
John’s Neck Alignment Evaluation
John, a 40-year-old software engineer, sought help for chronic neck pain and frequent headaches stemming from long hours at his laptop.
His therapist conducted a detailed neck alignment assessment, revealing key insights:
- Observation: John’s head posture showed a noticeable forward tilt, accompanied by rounded shoulders.
- Plumb Line Test: His ear was positioned nearly two inches forward of the plumb line, highlighting pronounced forward head posture (FHP).
- Craniovertebral Angle (CVA) Measurement: A CVA reading of 45° indicated a severe degree of FHP.
- Palpation: The therapist identified significant tightness in the upper trapezius and levator scapulae muscles, pointing to muscular imbalances.
Using these findings, the therapist created a personalized intervention plan involving cervical retraction exercises, ergonomic modifications, and targeted stretching such as scalene stretch.
Over three months, John experienced reduced pain, fewer headaches, and improved posture, underscoring the value of a meticulous neck alignment evaluation.
Scientific Backing for Neck Alignment Assessments
Research underscores the critical role of evaluating neck alignment in managing forward head posture (FHP).
Evidence-based techniques ensure accurate diagnosis and guide effective treatment plans:
- Journal of Orthopaedic & Sports Physical Therapy (2017): Demonstrated the reliability of craniovertebral angle (CVA) measurements for assessing FHP severity, linking smaller angles to increased postural deviations.
- Journal of Physical Therapy Science (2018): Highlighted the efficacy of the plumb line test in detecting forward head misalignment, offering a simple yet accurate diagnostic approach.
- Manual Therapy (2019): Emphasized functional movement testing as a key tool for identifying muscular imbalances and joint dysfunctions contributing to FHP.
These findings affirm the importance of thorough neck alignment evaluations.
Accurate assessments not only aid in diagnosing FHP but also improve treatment outcomes by targeting the root causes of postural issues.
The Value of Proper Assessment in Addressing FHP
Evaluating neck alignment is crucial for diagnosing and managing forward head posture (FHP).
This process identifies the severity and root causes of FHP, enabling therapists to create personalized intervention plans.
Techniques such as the plumb line test, craniovertebral angle (CVA) measurement, and palpation offer detailed insights into a patient’s posture, muscle imbalances, and joint dysfunctions.
These methods provide a foundation for targeted rehabilitation strategies.
In John’s case, a thorough assessment revealed significant FHP, which informed a tailored plan involving cervical retraction exercises and ergonomic adjustments.
Over three months, John experienced reduced neck pain, improved posture, and enhanced quality of life.
Research supports the efficacy of evidence-based tools in evaluating FHP, ensuring accurate diagnoses and effective treatment.
By addressing misalignments holistically, therapists can empower patients to achieve sustainable postural corrections, reducing symptoms and preventing future complications.
References: